One in two women will break a bone due to osteoporosis. For women, the risk of having osteoporosis is greater than their risk for heart attack, stroke and breast cancer combined.
Globally, an osteoporotic fracture occurs every three seconds.
Here’s what you need to know about osteoporosis.

Osteoporosis is a big problem
Osteoporosis means porous bone. Viewed under a microscope, healthy bone looks like honeycomb. But osteoporosis causes the holes and spaces in the honeycomb structure to become bigger, so bones are less dense. This thinning of bone structure makes a person’s bones weak, and they’re more likely to break.
Osteoporosis results in over 1.5 million fractures a year in the United States. In 2005, such fractures cost $19 billion.
The Surgeon General’s office published its first-ever report on Bone Health and Osteoporosis in 2004. The report says, “[B]one health is critically important to the overall health and quality of life of Americans.” It predicts that without significant action to address this issue, by 2020 (we’re almost there!) fully HALF of all Americans over age 50 would have or be at high risk for osteoporosis.
The National Osteoporosis Foundation puts it another way. Ten million Americans have osteoporosis. Another 44 million have low bone density. Together they make 54 million, meaning that half the adults over age 50 face greater risk of fracture and ought to be concerned about their bone health.
Risk Factors
The Mayo Clinic provides comprehensive patient information about osteoporosis. It discusses two categories of risk:
Unchangeable factors
- Gender – women are at greater risk than men
- Age – the older you are, the greater your risk
- Race – whites and Asians are at greater risk
- Family history – you’re at greater risk if you have a parent or sibling with osteoporosis, especially if a parent suffered a hip fracture
- Body frame size – a smaller body frame puts you at higher risk because you have less bone mass to draw on as you age
Factors you might be able to change
- Hormone levels – e.g. reduced estrogen in menopausal women
- Dietary issues – not enough calcium, eating disorder, gastrointestinal surgery
- Corticosteroids and other medications
- Medical conditions – e.g., celiac disease, cancer, lupus
- Lifestyle choices – sedentary lifestyle, tobacco smoke, excessive alcohol consumption

How do you know if you have osteoporosis?
Osteoporosis is silent – on your own, you can’t detect whether your bones are getting weaker over time. But it’s also common: one in two women and one in four men will have osteoporosis as they get older. The best way to determine whether you have osteoporosis is via a bone density scan.
DEXA scan
The most typical bone density scan is
Medicare covers DEXA scans for women over 65 and men over 70. If you’re over 50 and have had a recent fracture, your doctor will prescribe a scan and your insurance will usually cover it. Your doctor also might prescribe a DEXA scan because another factor (like corticosteroid use) places you at higher risk for osteoporosis.
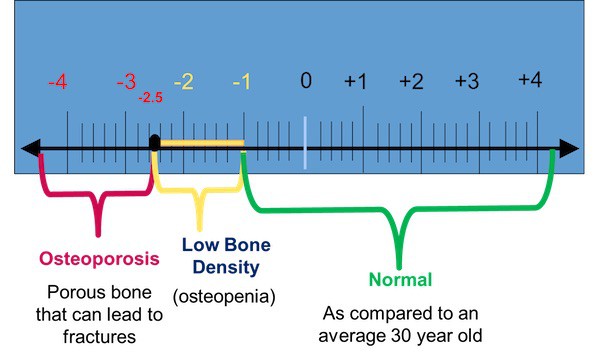
The DEXA scan generates your T-score, or measure of how your bone density compares to that of a healthy 30-year-old. T-score is a measure of standard deviation, but you don’t need to understand statistics to interpret your results.
The American Bone Health website has a useful diagram (reproduced below) that explains T-scores. If your T-score is 2.5 standard deviations from that of a healthy 30-year-old, you have osteoporosis.
Osteopenia
If your bone density falls between 1 and 2.5 standard deviations from that of a healthy 30-year-old, you have
How can you prevent osteoporosis?
The best way to prevent osteoporosis is to build bone density when you’re young. Peak bone mass occurs in girls at age 18 and boys at age 20. But even if you’re in midlife, there are still things you can do to build or preserve bone density.
Exercise
You’ve all heard about the importance of weight-bearing exercise for increasing your bone density. But what you may not know is that “weight-bearing exercise” isn’t limited to things like squats and kettlebells.
There are three types of exercise that matter for osteoporosis:
- Weight-bearing. This is any type of exercise where you move against gravity while remaining in an upright position. It includes high-impact activities like running, hiking and tennis. It also includes low-impact exercise like walking or using an elliptical or stair-step machine.
- Strength training. Exercises with weight machines, free weight and resistance bands increase your muscle strength. They don’t necessarily build bone density. But they can help prevent osteoporosis fractures by increasing your strength so you’ll avoid falls.
- Flexibility. As you grow older, your body grows stiffer. Having flexible joints is another way you can protect yourself from injury.

Yoga, Pilates and Ta’i Chi may help
Good news for people who like yoga. A 2016 Harvard Medical School study identified 12 yoga poses that, when done on a daily basis, helped to build bone density in addition to improving muscle strength, flexibility and balance.
Experts also consider Pilates and Ta’i Chi to be good for balance, flexibility and muscle strength. As such, they’re good low-impact exercises for people with low bone mass. Although their role in building bone density hasn’t yet been demonstrated, they, too, can help keep you from falling and breaking a bone.
Note that you should modify certain poses or exercises if you already have experienced osteoporotic fractures. Forward bends, for example, may further injure your neck. Always consult with your doctor before starting a new exercise program.
Swimming and cycling probably won’t help
Swimming and cycling, unfortunately, are not among the activities recommended to build bone density. They strengthen your muscles and build aerobic endurance. But in fact, studies of elite cyclists indicate such sports may lead to reduced bone density.
Mind your posture
Like your mom always told you: stand up straight. Correct posture holds your skeleton in good alignment, so there’s less stress on your spine. It also can limit kyphosis, or forward curve of the upper back – a condition that contributes to fractures in the upper vertebrae.
The National Osteoporosis Foundation has more information on proper body alignment on its website. It also posts diagrams showing you how you should modify exercises and routine body movements if you’re at risk for osteoporosis.

Diet
While you probably won’t increase your bone density with diet in midlife, make sure to eat so you’ll preserve the bone mass you have.
Calcium
The recommended calcium intake for women over 50 is 1200 mg/day. For men it’s 1000 mg/day. You can take a supplement for part of this amount. But your body absorbs nutrients best from food, not pills.
Dairy products are an ideal way to consume calcium. But there are lots of other calcium-rich foods. For example, kale, broccoli, certain types of fish, as well as fortified cereals and oranges give you calcium. Here’s a bigger list of foods that are rich in calcium.
Vitamin D
Vitamin D helps your body absorb calcium, and it supports your muscles as well. There are three ways to get Vitamin D:
- Sunlight. How much Vitamin D you absorb from the sun depends on things like skin pigmentation, latitude, season and whether you use sunscreen. Preventing skin cancer by using sunscreen is good. At the same time, using as low a sun protection factor (SPF) of 8 reduces Vitamin D production by as much as 95%.
- Food. There aren’t many foods that are rich in Vitamin D. You can eat wild-caught salmon, tuna and mackerel. Or try a Vitamin D-fortified milk, orange juice or cereal. Most people can’t get all the Vitamin D they need from food alone.
- Supplements. Because it’s hard to get enough Vitamin D from food or sunlight (especially if you use sunscreen), you probably should take a supplement. For more information about Vitamin D deficiency and supplements, check out this post.
Protein
One dietary element for increasing bone density that you might overlook is protein. But you need to eat protein along with calcium in order to build and maintain bone health.
Medication
If you’re diagnosed with osteoporosis, your physician may recommend medication. The most common osteoporosis drugs are bisphosphonates, which have brand names like Fosamax, Actonel, Boniva and Reclast. You’ve probably seen TV commercials for them.
Doctors may also prescribe osteoporosis medications for patients they deem to be at high risk – even if they don’t have an osteoporosis diagnosis. But the New York Times reported that in 2016, millions of Americans were missing out on potential benefits of osteoporosis drug therapies because they were terrified of the drugs’ rare side effects.
Bottom line: you need to evaluate your options, which include hormone replacement therapy and newer medications like Abaloparatide (brand name Tymlos) in addition to bisphosphonates. Consult with your doctor, do the research and choose the best course of action for your situation.

Increasing longevity means osteoporosis is rising
The older you get, the greater your risk of an osteoporosis-related fracture. This is especially true for post-menopausal women. Estrogen offers bone-protecting benefits throughout much of a woman’s life. But after menopause, bone breakdown overtakes the building of new bone.
So if you’re a midlife woman, what are your best chances for avoiding falls and fractures due to osteoporosis?
- Get a DEXA bone scan to know your baseline risk
- Eat a balanced diet that includes protein and calcium
- Take a Vitamin D supplement
- Do exercises that build bone density, muscle strength and flexibility
- Work on your balance and posture
- Consider medication if appropriate
Pay attention in the moment
Even if you’re doing all these things, you still might fall and break a bone. Don’t let bone density worries keep you from moving and doing the things you enjoy.
But do pay more attention. Personally, I’ve realized that the times when I’ve tripped have been times when I wasn’t focused on where I was going or what I was doing.
But I’m learning to be more aware. To slow down and focus on the present. There’s a bonus to this attitude. A lowered risk of fracture is only one of the benefits you can derive from attending to the here and now. After all, isn’t living in the moment considered a key to personal happiness? It’s a distinguishing characteristic of mindfulness meditation as well as other centering practices.
In some respects, then, it’s not so bad to be at an age where you face
Images via: Shutterstock, Pexels, Pixabay